MGUS Fatigue: Why You’re So Tired and How to Feel Better
Understanding MGUS Fatigue: What It Is, Why It Happens, and What You Can Do
A supportive guide to one of the most overlooked MGUS symptoms: extreme, lingering fatigue
If you’ve been diagnosed with MGUS—monoclonal gammopathy of undetermined significance—you probably left your doctor’s office with more questions than answers. You might’ve Googled it late at night, searched forums, or even found comfort in reading stories from others. But there’s one thing that keeps coming up in your day-to-day life that few seem to talk about: the sheer exhaustion.
Why am I so tired all the time? And could it be related to MGUS?
You’re not just imagining it. MGUS fatigue is a real symptom, and it’s one of the most frustrating ones. It doesn’t always show up in your lab results. You can sleep all night and still wake up drained. You might feel like you’re walking through molasses while everyone else is sprinting through their day.
This article is here to be your straight-talking, reassuring guide to understanding MGUS fatigue. We’ll explore why it happens, how it feels, what it might signal, and—most importantly—what you can do about it. Whether you’ve just been diagnosed or you’ve been quietly battling this for a while, this post will help you feel a little more seen, a little more informed, and a lot more empowered.
Does MGUS Really Cause Fatigue? Here’s What We Know
Let’s cut to the chase: yes, MGUS can cause fatigue—and no, it’s not all in your head.
At first glance, MGUS doesn’t seem like the kind of condition that would leave you feeling wiped out. It’s often described as “asymptomatic” or “harmless” by doctors. After all, it’s not cancer. So why do so many people living with MGUS report feeling utterly exhausted?
Here’s what’s going on under the hood:
-
Low-level inflammation: The abnormal proteins (called M-proteins) that MGUS produces may trigger subtle, ongoing inflammation in your body. And chronic inflammation? It’s a known energy zapper.
-
Mild anemia: Some MGUS patients have fewer healthy red blood cells. Less oxygen gets delivered throughout your body, which can leave you feeling sluggish, foggy, and short of breath.
-
Immune system disruption: Your immune system is working harder behind the scenes—sometimes on overdrive. That immune activation can quietly wear you down, especially if your body is constantly playing defense.
-
Mental and emotional fatigue: Let’s not overlook the stress factor. Living with MGUS means regular monitoring, scary-sounding terms, and the constant question: “Could this turn into cancer?” That worry alone can quietly drain your battery.
If you’ve ever wondered, “Does MGUS cause fatigue?” or “Why am I so tired with MGUS?”—you’re asking the right questions. And you deserve real answers, not brush-offs.
MGUS is often described as “asymptomatic” or “harmless” by doctors—according to the Mayo Clinic’s overview on MGUS—but the fatigue some people experience tells another story.
Have your provider check for nutrient deficiencies—especially Vitamin D. Here’s why Vitamin D deficiency can cause fatigue, even in seemingly healthy people.
What MGUS Fatigue Feels Like (and Why It’s Different from Being Just Tired)
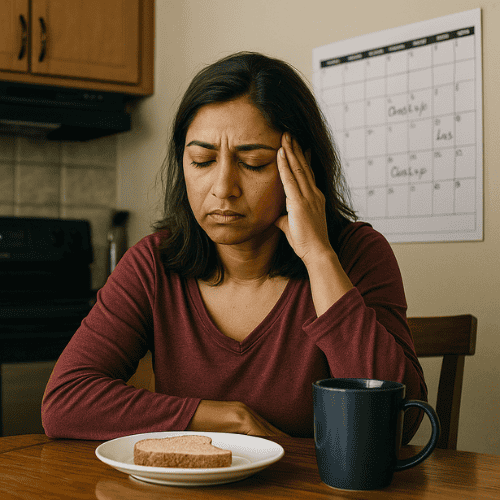
We all know what it’s like to feel tired after a long day or a bad night’s sleep. But MGUS fatigue? That’s a different beast altogether.
This kind of tiredness doesn’t play fair. It lingers. It sneaks into your bones. And worst of all? It doesn’t always make sense. You could get a full night’s rest and still wake up feeling like you’ve run a marathon in your sleep.
Here’s how people often describe fatigue from MGUS:
“It’s like moving through molasses.” Even simple tasks—like doing the laundry or running errands—can feel strangely overwhelming.
Brain fog creeps in, making it harder to focus or remember small things.
Muscle heaviness or weakness shows up, even when you haven’t exercised.
You might feel lightheaded or winded after mild activity.
And maybe you feel like your battery drains faster than it used to—like you only get a few “good” hours each day before the crash.
Does any of that sound familiar?
Fatigue and monoclonal gammopathy aren’t always mentioned together in a diagnosis conversation, but many MGUS patients experience exactly this kind of slow-burn exhaustion. Learn more about other subtle symptoms in Understanding MGUS Symptoms: A Comprehensive Look at Early Signs and Health Monitoring.
Because here’s the truth: this isn’t just regular tiredness—it’s a signal.
How to Manage MGUS Fatigue (Without Losing Your Mind)
There’s no magic switch to turn off MGUS fatigue—but there are real, practical ways to turn down the volume on it. The key is figuring out what’s draining your energy and building small habits that help you get some of it back.
Here are smart, manageable strategies that many people with MGUS find helpful:
1. Track Your Energy Like a Detective
Keep a simple fatigue log. Each day, jot down:
What time you woke up and how you slept
Meals and snacks
Activities and energy dips
Any symptoms like brain fog, shortness of breath, or muscle aches
2. Move Your Body (Gently)
It sounds counterintuitive, but light movement can actually help restore energy over time. Start with:
A 10–15 minute walk
Gentle stretching or beginner yoga
Standing and moving during screen time or chores
Even small bursts of activity increase circulation, lift your mood, and support healthier blood flow—all important when managing a blood disorder.
3. Rule Out Sneaky Culprits
Ask your care team to check for:
Anemia
Vitamin D or B12 deficiency
Thyroid issues
Sleep apnea or poor-quality rest
These can pile onto MGUS fatigue or mimic it altogether. Treating one of these may ease your tiredness significantly.
4. Eat to Recharge
Think of food as fuel, not just filler. An anti-inflammatory diet helps stabilize energy and reduce stress on your immune system. Curious about natural anti-inflammatory options? Check out Turmeric and MGUS: Can Curcumin Help Support Your Immune System Naturally. Focus on:
Leafy greens, berries, and veggies
Lean protein like fish or legumes
Whole grains and healthy fats
Plenty of water

Limit added sugars, alcohol, and ultra-processed foods—they’re energy thieves. These foods may give you a quick boost, but they often lead to a crash that worsens your MGUS fatigue. Instead, focus on consistency and whole-food nourishment throughout the day.
Want a shortcut? Our post on Green Drinks and MGUS breaks down which smoothies or powders may help you boost energy naturally.
5. Have the Talk With Your Doctor
Don’t just push through. Fatigue might seem like “part of the deal,” but it can signal something changing in your health. Try saying:
“I’ve been feeling unusually fatigued. Could we review my latest labs and talk about possible causes or next steps?”
They may adjust your follow-up schedule, recommend lifestyle tweaks, or run extra tests to be sure everything’s staying stable.
When to Worry: Could Your Fatigue Mean MGUS Is Progressing?
Most of the time, MGUS fatigue is annoying—but stable. However, if your exhaustion feels worse than usual, suddenly ramps up, or comes with new symptoms, it’s worth pausing and asking: Is something changing?
While fatigue alone doesn’t confirm MGUS is progressing to something more serious (like smoldering multiple myeloma or multiple myeloma), it can sometimes be one of the first signs that your body needs a closer look.
Red Flags to Watch For
Talk to your doctor if your fatigue shows up alongside:
New or worsening bone pain (especially in the back, ribs, or hips)
Frequent infections or taking longer to recover from colds or bugs
Unexplained weight loss or appetite changes
Persistent anemia or low blood counts in recent labs
Elevated M-protein levels or changing lab markers
Numbness or tingling in your hands, feet, or legs
These signs don’t automatically mean MGUS is progressing—but they do mean it’s time to speak up and potentially order updated tests.
What Your Doctor Might Check
If there’s concern about progression, your care team may order:
Repeat bloodwork (especially for M-protein levels, calcium, and free light chains)
Urine tests (looking for Bence Jones protein)
Bone marrow biopsy (if needed to check plasma cell counts)
Imaging tests like X-rays, MRIs, or PET scans to look for bone lesions
Catching progression early can dramatically improve your outcome—so don’t wait if something feels “off.” You’re not overreacting; you’re advocating.
Fatigue Might Be Part of MGUS—But It Doesn’t Have to Run the Show
Let’s be honest: when you’re wiped out by noon and running on fumes, it’s easy to feel frustrated, defeated, or even scared. Especially when your labs don’t show anything “urgent,” but your body is clearly waving a red flag.
Here’s the truth you need to hear:
MGUS fatigue is real. It’s not in your head, it’s not weakness, and you’re not alone.
Yes, it can be tied to the condition itself—through inflammation, anemia, or immune system changes.
Yes, it can be worsened by stress, sleep problems, or other hidden culprits.
And yes, there’s something you can do about it.
You don’t have to settle for dragging through your days.
Instead, take these empowering steps:
Start tracking your symptoms and lab trends
Move gently and often, even on low-energy days
Fuel your body with whole foods and hydration
Speak up at appointments and ask better questions
Look at the whole picture—not just numbers on a chart
Because managing MGUS means more than “watchful waiting.” It means paying attention, making small shifts, and staying informed so you can feel like you again.
Read our companion article MGUS Test Results Explained — a clear, friendly guide to interpreting your labs and starting stronger conversations with your care team.
You deserve answers.
You deserve support.
And most of all—you deserve to feel better.
