MGUS Test Results Explained: A Friendly Guide to Understanding Your Labs and What Comes Next
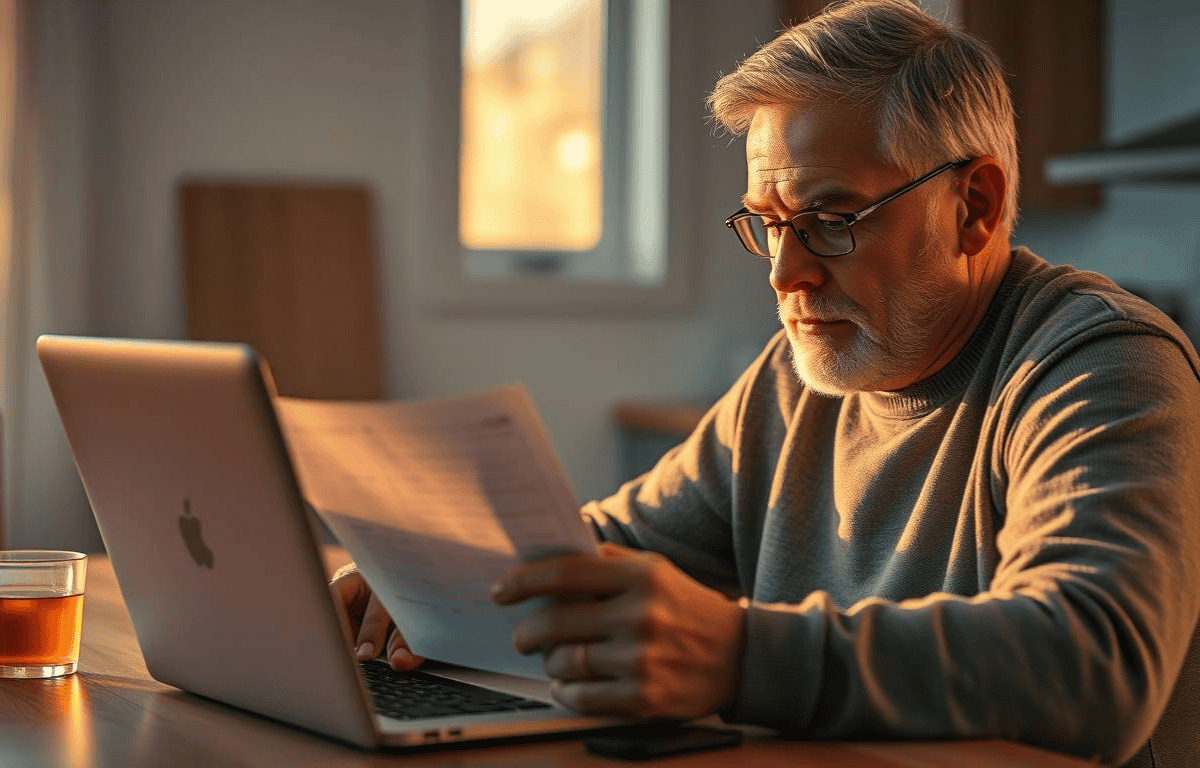
The Lab Report Just Hit Your Inbox — Now What?
You open your email, and there it is: “Your MGUS test results are ready.”
You click. You scroll. You stare. Suddenly, it feels like you’ve landed in the middle of a medical crossword puzzle you didn’t sign up for.
What’s an M-spike? Why are there three immunoglobulin letters? And do those numbers mean something terrible… or are they just your blood’s way of saying, “Hey, I’m doing something funky, but I’m not cancer (yet)?”
If this sounds familiar, you’re not alone. MGUS (Monoclonal Gammopathy of Undetermined Significance) can feel like a diagnosis wrapped in a riddle. The good news? It’s not cancer. The not-so-great news? It’s not nothing either. It’s a blood condition that needs watching. And those test results? They’re your roadmap.
This guide is here to help you unpack those labs, explain them like we’re chatting over coffee, and give you the confidence to know what’s normal, what’s not, and what questions to ask your doctor.
No jargon. No panic. Just clear, supportive info to help you take control of your MGUS journey.
✨ Want to support your immune health while monitoring MGUS? Many people explore natural anti-inflammatory options like this top-rated turmeric supplement on Amazon. (Always talk to your doctor before starting new supplements.)
Ready? Let’s crack the code on your bloodwork together.
Cracking the Code — Common MGUS Lab Terms
Let’s be honest: MGUS lab reports can look like they were written in a secret language designed to confuse you. So let’s break it down. Below are the key terms you’ll see in your test results—decoded in plain English.
🧪 M-Spike (Monoclonal Spike)
This is the main marker that shows up in a serum protein electrophoresis (SPEP) test. It reflects how much monoclonal protein (or “M protein”) is in your blood.
A normal M-spike is 0.
With MGUS, it’s usually less than 3.0 g/dL.
A rising M-spike can suggest a need for closer monitoring.
Want a deeper dive into what this means for your risk? Check out our post: MGUS and Cancer: Is It Inevitable?
⚖️ Free Light Chains (Kappa & Lambda)
These are fragments of antibodies. The important part here is the kappa/lambda ratio:
A normal ratio ranges from 0.26 to 1.65.
Ratios outside this range might suggest a higher risk of progression.
Want to track these values easily at home? A simple health log notebook like this one can help you keep notes for your next doctor’s visit.
📊 Quick Lab Value Summary
| Test | Normal Range | MGUS Flag |
|---|---|---|
| M-Spike | 0 g/dL | < 3.0 g/dL |
| IgG | ~700–1600 mg/dL | Often elevated |
| Free Light Chain Ratio | 0.26–1.65 | May be skewed |
| IgA or IgM | Varies | Usually low or normal unless subtype |

How to Read Your MGUS Test Results Without Freaking Out
You’ve got your lab results in hand—maybe from Quest, Labcorp, or directly through your doctor’s portal. The numbers, symbols, and strange abbreviations are all there… and suddenly, so is the panic.
Take a deep breath. You don’t need to be a medical expert to make sense of your MGUS labs. You just need to know what to look for, and more importantly—what not to worry about.
🧭 Step 1: Spot the M-Spike
This is the headline item from your SPEP test (Serum Protein Electrophoresis).
If your M-spike is under 3.0 g/dL, you’re still in MGUS territory.
If it’s inching upward or over that threshold, your doctor may run further tests to rule out progression.
Want to track how your M-spike has changed over time? Use a durable health log like this one to keep things organized and ready for your next appointment.
📊 Step 2: Review Your Immunoglobulin Levels
Look for IgG, IgA, or IgM in your test report. One of them will be higher—this is the antibody type producing your monoclonal protein.
IgG MGUS = most common and typically lowest risk
IgM MGUS = linked to different progression paths
IgA MGUS = intermediate risk and may need more frequent follow-up
Learn more about these subtypes and what they mean in MGUS IgM Explained: Steps to Clarity & Care.
⚖️ Step 3: Check the Kappa/Lambda Ratio
This is part of the Free Light Chain assay, and it’s a critical indicator.
A normal ratio ranges from 0.26 to 1.65
A ratio outside this range doesn’t always mean something serious—but it does prompt your doctor to watch more closely over time
📝 Step 4: Focus on Trends, Not One-Time Results
This is the part many doctors forget to explain: MGUS is all about the long game.
One strange number is not a reason to panic
Slight fluctuations are normal
Your doctor is mostly watching for consistent upward trends, not isolated blips
💬 Bonus Tip: Bring Questions to Your Appointments
Even if you’re unsure what everything means, don’t hesitate to ask. Try questions like:
“Is my M-spike stable compared to last time?”
“Which type of MGUS do I have?”
“Is this light chain ratio something we’re monitoring closely?”
Monitoring MGUS Over Time: What Changes and What Matters
So, you’ve decoded your test results. You know what an M-spike is, you’ve figured out the kappa/lambda ratio, and you’re doing your best not to obsess over the numbers. Now comes the next chapter: monitoring—a long-term partnership with your bloodwork that helps spot changes before they become problems.
This isn’t about living in fear—it’s about staying informed, paying attention to trends, and working with your doctor to stay one step ahead.
How Often You’ll Get Tested
For most people with MGUS, blood tests are repeated every 6 to 12 months, depending on risk level.
Low-risk MGUS? Annual testing may be enough.
Higher-risk MGUS? You may be monitored every 3–6 months, especially if your M-spike or light chain ratio begins to shift.
When Should You Be Concerned? Understanding Risk Factors
It’s totally normal to wonder, “Is this going to turn into something serious?” The word “precancerous” isn’t exactly calming. But before you let your imagination run wild, let’s look at the facts.
The Reality: Most People with MGUS Never Develop Cancer
Studies show that MGUS progresses to multiple myeloma or a related disorder at a rate of about 1% per year. That means after 10 years, 90% of people still only have MGUS. Many live long, healthy lives with regular checkups and nothing more.
Still, certain test results can indicate a higher risk of progression. This is where “risk stratification” comes in—and where your doctor may adjust how often you’re monitored.
Key Risk Factors That May Raise Eyebrows
Your doctor will keep a close eye on a few specific indicators:
M-spike over 1.5–2.0 g/dL
Even if you’re still under the 3.0 g/dL MGUS threshold, anything steadily climbing above 1.5 may require more frequent follow-ups.
Non-IgG subtype (IgA or IgM MGUS)
Most people are diagnosed with IgG MGUS, which typically carries the lowest risk. However, if your results point to IgA or IgM, your doctor may take a closer look, as these subtypes are monitored a bit differently and may carry a slightly higher potential for progression.Abnormal Free Light Chain Ratio
Ratios far outside the normal range (0.26 to 1.65) could suggest more aggressive plasma cell activity.Low Normal Immunoglobulin Levels (Suppression)
If your body isn’t producing enough healthy antibodies alongside the monoclonal ones, it may signal a higher-risk profile.
Still unsure about your risk category? The Mayo Clinic’s overview of MGUS provides a great breakdown of risk factors and progression rates.
MGUS and Cancer — Is It Inevitable?
Let’s tackle the question everyone with MGUS secretly Googles: “Does this mean I’m going to get cancer?”
Short answer: No.
Longer answer: MGUS is not cancer. It’s a condition that could turn into cancer, but usually doesn’t.
Why MGUS Gets Linked to Cancer
MGUS is considered a precancerous plasma cell disorder because it can progress to:
Multiple myeloma (the most common)
Waldenström’s macroglobulinemia
AL amyloidosis
But progression isn’t guaranteed. According to the National Cancer Institute, most people with MGUS never develop these conditions.
In fact:
After 5 years, 95% still only have MGUS
After 10 years, 90% still do
Even after 20 years, the majority haven’t progressed
That’s a pretty solid track record for a condition that gets such a scary reputation. It reminds us that MGUS is often more of a watch-and-manage situation than an urgent medical crisis.
MGUS Is a Red Flag, Not a Red Alert
Think of MGUS like your body’s check engine light. It’s not saying something is broken—it’s saying, “Let’s pay attention and check this periodically.”
That’s why monitoring matters. Not because you’re destined for something worse, but because if something changes, your doctor can catch it early.
If you want to learn more about how MGUS relates to multiple myeloma, we break that down in MGUS and Multiple Myeloma: Understanding the Link and What Comes Next.
Feeling anxious after reading about all this? Many people find that building a supportive lifestyle helps calm the nerves between lab visits. Consider daily stress support supplements like ashwagandha or magnesium glycinate—just be sure to talk with your doctor first.
(These aren’t cures but may help you feel more balanced while living with MGUS. Always check with your healthcare provider.)
Can My Results Change Over Time? Yes — and That’s Okay
You’ve had your first MGUS lab results. You’ve done the Googling. You’re breathing a little easier.
Then the next round of bloodwork comes in… and something’s changed. A value’s a little higher. A ratio’s a little off. You start to wonder: Is this it? Is this the start of something worse?
Let’s pause right there.
Blood Test Results Are Like Snapshots
Your lab numbers are a moment in time. And just like your weight can fluctuate after salty food or a bad night’s sleep, your MGUS markers can shift slightly without meaning anything serious.
Here’s what can cause natural variation:
Minor illness (even a cold can nudge your immune numbers)
Dehydration
Time of day your blood is drawn
Lab calibration differences
Your M-spike might inch up, or your light chain ratio might tilt a bit—and that’s normal. It doesn’t mean progression. It means your body is doing what bodies do: ebb and flow.
What Your Doctor Is Really Watching
Your hematologist isn’t focused on one odd result—they’re looking for patterns over time:
Is your M-spike climbing steadily, not just spiking once?
Is your kappa/lambda ratio trending further out of range?
Are there new symptoms developing alongside the lab changes?
Want a deeper understanding of the “watch and wait” process? Visit MGUS Diagnosis Demystified: Unlocking Your Health Journey for a full breakdown of how your condition is tracked.
Say “continue” when you’re ready for the final section: You’re Not Alone — Understanding Is the First Step.
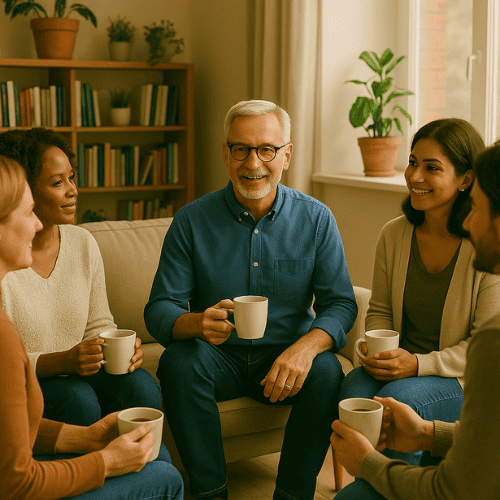
You’re Not Alone — Understanding Is the First Step
If you’ve made it this far, take a deep breath—and a bit of pride. MGUS can feel like an overwhelming acronym dropped into your life without warning. But now you understand what it is, how to read your results, and what to look for moving forward.
Here’s what we hope you’re taking away:
You don’t have to panic over every lab result
Monitoring MGUS is about trends, not one-time numbers
Most people with MGUS never develop cancer
There are steps you can take to feel more confident and in control
What You Can Do Right Now
You don’t need to memorize every lab abbreviation. You just need a plan. Try these simple steps:
Keep a copy of each blood test so you can compare over time
Track changes using a dedicated health journal
Write down questions before your doctor visit (so nothing gets forgotten)
Consider lifestyle support, like turmeric supplements for inflammation or vitamin D3 if your levels are low
And remember: you’re not doing this alone.
Our blog is here to help you navigate this MGUS journey—whether you’re newly diagnosed or months into monitoring. You’ve got this.
And if this post helped you, consider sharing it with someone who needs clarity, too.
We’re in your corner. 💚
